
Safe hands at Christmas time
Hand hygiene is the key to ensuring the safety of guests and the success of the menu. Have an enjoyable time, celebrate and eat without the risk of food poisoning!

On this occasion, the blog ‘The Dirt on My Hands’ addresses hand hygiene from a health perspective, with a specific focus on nursing homes and geriatric centres. We reflect on how incorrect hand hygiene increases the risk to the health of our elderly, who are extremely vulnerable to nosocomial infections.
We analyse the main routes of pathogen transmission, highlighting the role of healthcare technicians. We also emphasised the importance of promoting a culture of responsibility and prevention, demonstrating that a practice as simple as hand washing can make a difference to the quality of care and prevent infectious outbreaks in care homes and nursing homes.
In addition, we underline the need to implement rigorous hygiene protocols, training programmes and awareness campaigns for at-risk environments with vulnerable users.
In nursing and care homes, hands are one of the main routes for the transmission of infections. Although they may appear clean, they can harbour all kinds of dirt. Identifying what kind of contaminants can be accumulated is the first step to understanding why good hygiene is not optional, but vital.

There are two main kinds of dirt on hands:
Visible or mechanical soiling:
This is the most obvious: traces of food, body fluids, soil, dust, secretions or any particles that can be seen with the naked eye. In a geriatric setting, this can include anything from residue from dressings or creams to biological debris such as mucus or faeces after toileting.
Invisible or microbiological dirt:
This is the most dangerous and often the most overlooked. These are bacteria, viruses and fungi that cannot be seen but are transmitted. Some common examples in geriatrics include Staphylococcus aureus, E. coli, Clostridium difficile or even influenza virus or SARS-CoV-2. These can adhere to the skin after contact with contaminated surfaces, people, utensils, or during routine procedures such as changing a nappy or taking a blood pressure.
In addition, there is a third implicit type:
Soiling due to carelessness or negligence:
It is the most difficult to eradicate: lack of proper washing or the time needed, misuse of gloves or forgetting to disinfect after contact with residents or their belongings. It is invisible while it leaves its mark in the form of infections.
About healthcare-associated infections, according to the Spanish Society of Preventive Medicine, Public Health and Health Management, the scientific society that promotes the Study of the Prevalence of Nosocomial Infections in Spain (EPINE), they cause 7,414 deaths annually in Spain and cause direct costs of €2,025 million. In addition, data from this study, in 2023, indicate that the prevalence of having a healthcare-associated infection in hospitalised patients aged 70 years or older was 10.02%.
Data from the PRINCESS programme for infection prevention in health care centres.
Residents in private residential centres or social services for the elderly present a high risk of acquiring infections, not only because of their vulnerability due to their age, frailty and limited autonomy but also because of the large presence of comorbidities and polymerization, where there is a higher risk of adverse effects and interactions associated with the prescription of antimicrobials and because of the characteristics of these centres.

In addition, the frequent use of external devices and the fact that they share common objects, areas and caregivers facilitates the acquisition, development and cross-dissemination of multi-resistant microorganisms, making the infection incidence high in these centres. For all these reasons, it is considered relevant to promote and apply prevention and control programmes in nursing homes and social and healthcare centres to reduce Healthcare Associated Infections (HCAI), also known as nosocomial infections.

These five pillars summarise the keys to ensuring effective, sustained, and safe practice. Training, standard setting, resourcing, monitoring and awareness are essential to protect those who need it most.
Infrastructures and resources. In order to carry out a hand hygiene improvement programme. It is essential to have with the existence of adequate infrastructures and resources, among which we highlight: individual alcohol-based products for workers and for common use by family members and residents of the centre. Adequate facilities for hand washing with water, alcohol-based products (ABP) or soap dispensers and paper towels.
Training and coaching of staff. Recognise the completion of training on a nominative basis (competence verification system). Staff training (at the moment of incorporation and repeated periodically, at least once a year) following the WHO model of the 5 moments, adapted to 4 moments for socio-health and geriatric centres.
Programme evaluation. Identify successful outcomes and foster collaborative learning. To highlight opportunities for improvement to focus new actions.
Reminders in strategic areas of the workplace. In poster form and information leaflets in areas where there may be a risk of cross-transmission of micro-organisms, such as medication preparation rooms, treatment rooms, physiotherapy rooms, etc.
Foster a good safety climate. It is essential to create an environment in which everyone involved is made aware of the importance of hand hygiene for the safety of everyone: workers, residents and family members.
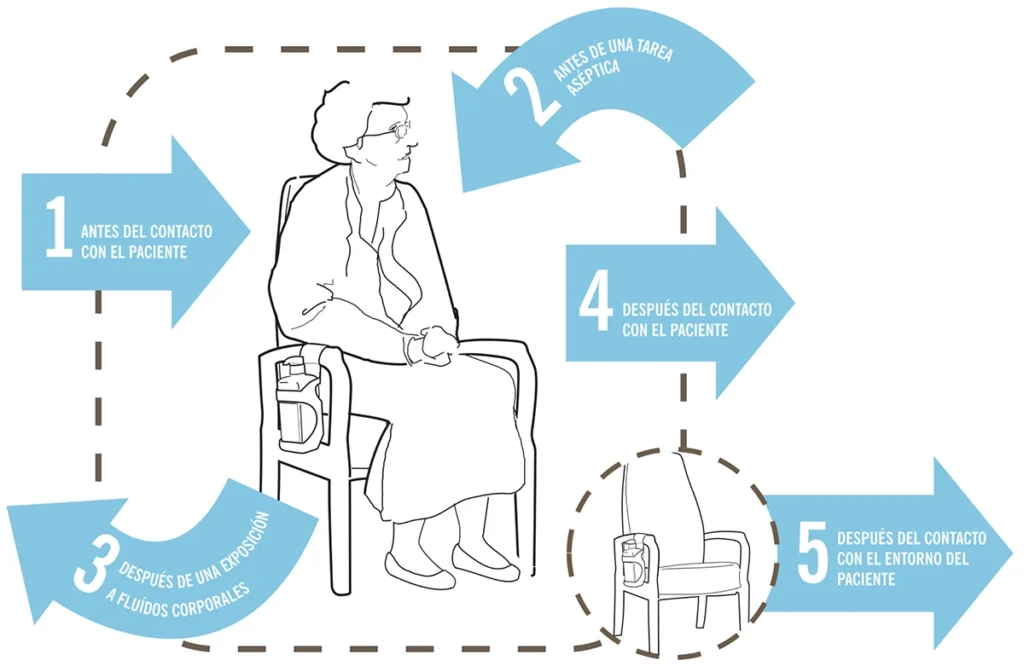
WHEN: Perform hand hygiene before touching the patient, when approaching the patient.
EXAMPLES: Shaking hands, helping the patient to move, performing a clinical examination.
1
BEFORE CONTACT WITH THE PATIENT
WHEN: Perform hand hygiene immediately before any aseptic task.
EXAMPLES: Oral/dental care, aspiration of secretions, dressings, insertion of catheters, preparation of food or medication.
2
BEFORE AN ASEPTIC TASK
WHEN: Immediately after possible exposure to body fluids and (after removal of gloves).
EXAMPLES: Oral/dental care, aspiration of secretions, collection and handling of blood, urine, faeces, waste handling.
3
AFTER EXPOSURE TO BODY FLUIDS
WHEN: Perform hand hygiene after touching the patient or his or her immediate environment when moving away from him or her.
EXAMPLES: When shaking hands, helping the patient to move, performing a clinical examination.
4
AFTER CONTACT WITH THE PATIENT
WHEN: After touching any object or furniture in the patient’s immediate environment (even if the patient has not been touched).
EXAMPLES: Changing bed linen, adjusting perfusion rate.
5
AFTER CONTACT WITH THE PATIENT’S ENVIRONMENT
We share with you a series of resources to raise awareness and train users and workers, whatever your area of business or workplace. We put at your disposal the WHO posters to remove dirt from hands and disinfect them, as well as the moments of hand hygiene, both in the health and social-health fields and in nursing homes or geriatric homes.
The right products to remove dirt on your hands depend on the type of dirt (visible or invisible) and the context. Here is an overview of the best options for keeping skin clean, healthy and safe:
Furthermore, implementing appropriate dosing systems ensures and promotes good personal hygiene practices in any collective setting.
1. Soap and water (preferably lukewarm).
2. Alcohol-based solutions (lotion/gel).
PRODERPHARMACARE® works to offer formulations that remove dirt from hands. Below we recommend the products that meet the needs of hand washing and antisepsis while caring for the skin of users and professionals in health centres, socio-health centres, nursing homes and geriatric homes.

Hand hygiene is the key to ensuring the safety of guests and the success of the menu. Have an enjoyable time, celebrate and eat without the risk of food poisoning!

PRODERPHARMACARE® attends Hygienalia 2025 with an impeccable presentation, where product testing has been the main attraction.